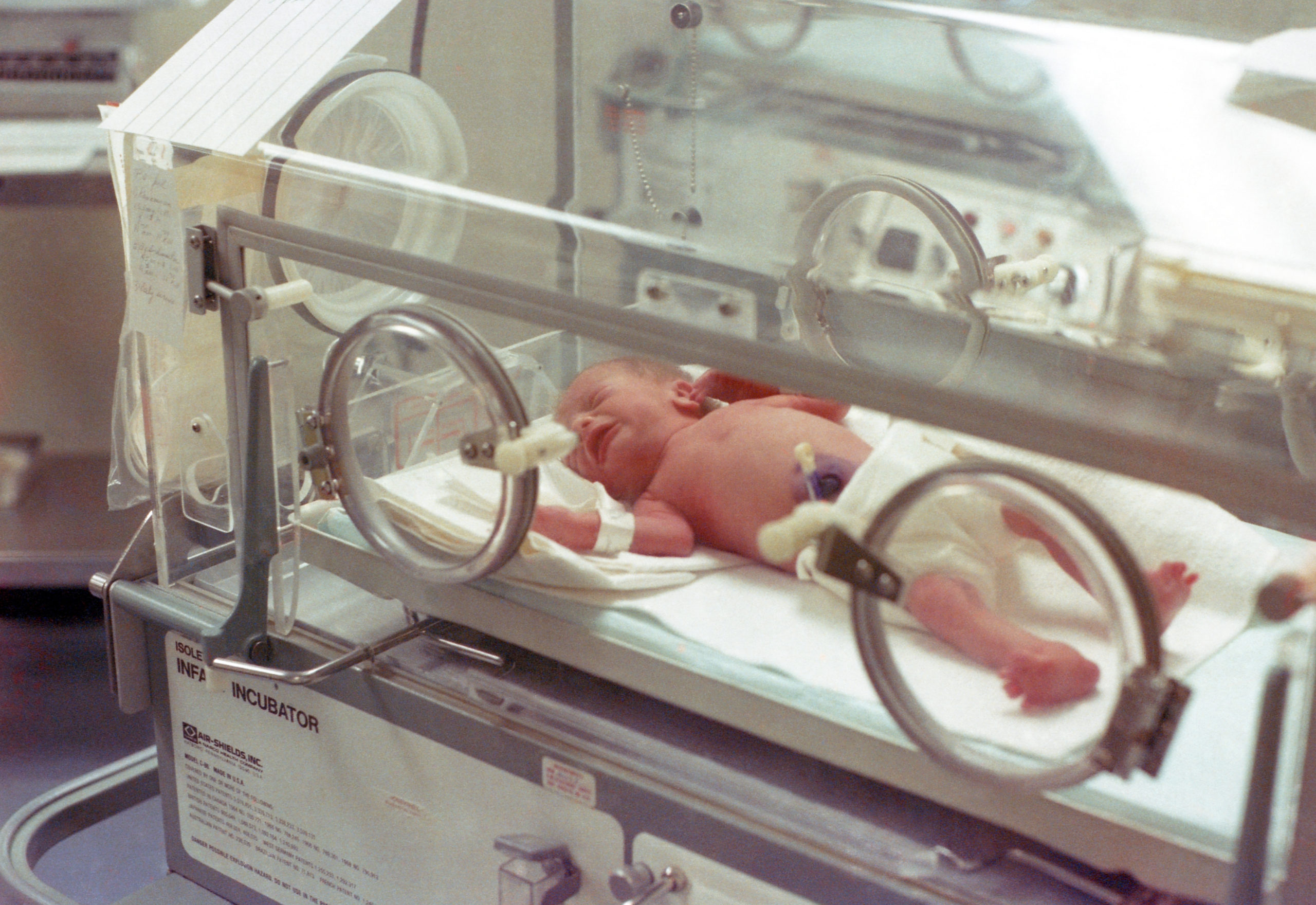
Babies being discharged from the NICU face higher risks for medical and developmental issues than their peers. For this reason, it’s critical for providers to establish and enforce follow-up protocols that meet each baby’s specific care needs.
To prepare parents of neonates to take their babies home after being discharged from the NICU, hospitals and healthcare organizations use programs with recommendations for home life and follow-up care. For instance, the National Association of Neonatal Nurses has put together a program titled “Baby Steps to Home,” which features guidelines for follow-up care for neonates for both parents and NNPs. While recommendations may vary slightly from one health care system to the next, here’s a general look into follow-up care guidelines for babies who have been discharged from the NICU.
Typical Schedule of Visits
The specific schedule of follow-up care visits will be based on each child’s specific needs. In general, however, visits are scheduled at three, six, 12, 18, and 24 months. In most cases, NNPs care for neonates, infants, and toddlers up to age two.
Additionally, keep in mind that visits are scheduled based on the infant’s adjusted age if they were born prematurely. For instance, children born at 28 weeks (or three months prematurely) may not have their first visit until they’re three months old in corrected age, which would actually be six months chronologically from birth.
What Follow-Up Care Entails
Each follow-up appointment is tailored to children’s specific needs. In general, neonatal follow-up visits may include:
- A thorough physical examination and discussion of health history. NNPs may discuss medical history, any recent illnesses or medical issues, and medications. Providers will also perform a physical and neuromotor evaluation and check the child’s vital signs.
- Growth checks
- Screening for early signs of developmental concerns, such as autism
- Nutritional counseling
- Evaluation of possible needs for additional services, such as speech or physical therapy
- Coordination of care with the child’s pediatrician
- Referrals for specialists, if needed
In many cases, follow-up care for neonates calls for a multidisciplinary approach which can involve a number of specialists. According to the World Health Organization Collaborating Center for Training and Research in Newborn Care, neonatologists and pediatricians may serve as the core providers, but follow-up care may encompass visits to other specialists. For instance, the following team members are often involved in follow-up care for neonates:
- Child psychologists, who screen for behavioral issues and perform formal neurodevelopmental assessments
- Pediatric neurologists, who can help to manage issues such as seizures or other neurological illnesses over a long-term basis
- Ophthalmologists, who test visual acuity and screen for potential issues
- Otorhinolaryngologists, who perform hearing assessments and manage any impairments, if needed
- Dieticians, who provide tailored dietary advice and manage the diets of infants and children with special needs
- Physiotherapists, who assess muscle tone and power and provide training programs if needed
- Speech/occupational therapists, who offer rehabilitation for infants with impairments and disabilities
As an NNP, you may find yourself communicating not only with the parents of neonates, but also specialists across several medical disciplines. Having this comprehensive understanding of follow-up care can help you provide quality care for neonates from the moment they’re born through their early toddler years.
If you’re seeking a job as an NNP, allow our specialists to help you take the next step to further your career. From relocation support to Locum Tenens placement, our team can recommend employment options that fit your wants and needs. Get started with a free career consultation.