It is with great honor and respect I introduce to you our guest presenter for this month – Dr. Suzanne Staebler. Suzanne has a bio which is almost unrivaled. In addition to being widely published, a prominent invited lecturer, and having held numerous roles on NANN & NANNP Leadership Committees Suzanne brings to our profession an enthusiasm and zest for neonatal nursing which is rarely matched. Suzanne received her MSN / NNP in 1991 and DNP in 2010. She has worked not only in staff NNP capacities but in teaching, consulting and leadership roles as well. Her most recent venture being to head up the newly opened NNP program at the Emory University School of Nursing in Atlanta. I am proud to also call her my friend. — Tim Mattis
As the implementation of the Affordable Care Act (ACA) continues to roll out, there is more national attention focusing on advanced practice nurses (APRNs). Recently, June 18, 2013, there was a WSJ article regarding the ability of nurse practitioners and other APRNs (CRNAs- certified registered nurse anesthetist; CNM- certified nurse midwife) to provide high-quality, safe and cost-effective care. As the physician shortage continues to grow, and those in the medical workforce shrink (as many who are near retirement), the healthcare system must consider the vital role of these APRNs in care delivery.
What are the different types of APRNs?
1. Nurse Practitioner
Nurse practitioners (NP) are members of the health delivery system, practicing autonomously in areas as diverse as family practice, pediatrics, internal medicine, geriatrics, neonatology and women’s health care. NPs are prepared to diagnose and treat patients with undifferentiated symptoms as well as those with established diagnoses. Both primary and acute care NPs provide initial, ongoing, and comprehensive care, includes taking comprehensive histories, providing physical examinations and other health assessment and screening activities, and diagnosing, treating, and managing patients with acute and chronic illnesses and diseases.
This includes ordering, performing, supervising, and interpreting laboratory and imaging studies; prescribing medication and durable medical equipment; and making appropriate referrals for patients and families. Clinical NP care includes health promotion, disease prevention, health education, and counseling as well as the diagnosis and management of acute and chronic diseases. Certified nurse practitioners are prepared to practice as primary care NPs and acute care NPs, which have separate national consensus-based competencies and separate certification processes.
2. Certified Registered Nurse Anesthetist
The Certified Registered Nurse Anesthetist is prepared to provide the full spectrum of patients’ anesthesia care and anesthesia-related care for individuals across the lifespan, whose health status may range from healthy through all recognized levels of acuity, including persons with immediate, severe, or life-threatening illnesses or injury. This care is provided in diverse settings, including hospital surgical suites and obstetrical delivery rooms; critical access hospitals; acute care; pain management centers; ambulatory surgical centers; and the offices of dentists, podiatrists, ophthalmologists, and plastic surgeons.
3. Certified Nurse Midwife
The certified nurse-midwife provides a full range of primary health care services to women throughout the lifespan, including gynecologic care, family planning services, preconception care, prenatal and postpartum care, childbirth, and care of the newborn. The practice includes treating the male partner of their female clients for sexually transmitted disease and reproductive health. This care is provided in diverse settings, which may include home, hospital, birth center, and a variety of ambulatory care settings including private offices and community and public health clinics.
4. Clinical Nurse Specialist
The CNS has a unique APRN role to integrate care across the continuum and through three spheres of influence: patient, nurse, system. The primary goal of the CNS is continuous improvement of patient outcomes and nursing care. Key elements of CNS practice are to create environments through mentoring and system changes that empower nurses to develop caring, evidence-based practices to alleviate patient distress, facilitate ethical decision-making, and respond to diversity.
(Definitions taken from Consensus Model for APRN Regulation: Licensure, Accreditation, Certification & Education, 2008; downloaded from https://www.ncsbn.org/4213.htm )
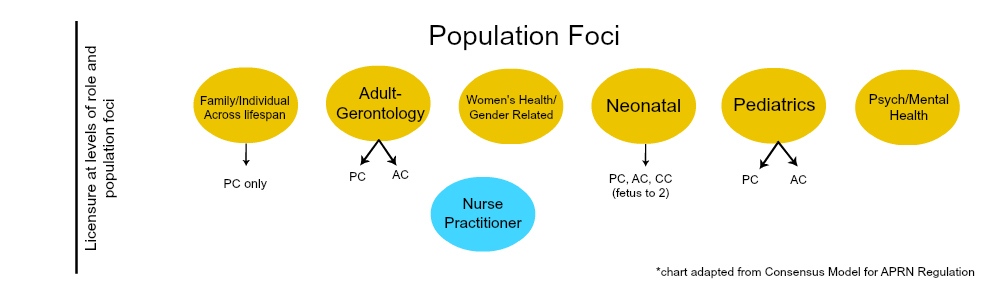
Scope of practice for APRNs is a blend of their educational preparation, their board certification and state level regulations. For nurse practitioners, this can get a bit blurry as they are educated in a specific population of specialization (adult-gerentology; pediatrics; neonatal; psyche-mental health, women’s health and family health); In pediatrics and adult populations, NPs further specialize into primary care (health wellness and promotion; chronic disease management) and acute care (ranging from acute episodic care to critical care);
To determine scope of practice for APRNs, consideration must be given to advanced practice education in a role and population foci, scope of practice standards published by the national specialty organization or APRN associations, and the state’s nurse practice act and board of nursing rules and regulations. For most boards of nursing, the scope of practice for the APRN is based upon his or her advanced educational preparation (NCSBN, 2012).
The patient population, advanced educational program content, and competencies obtained in the advanced practice nursing educational program always serve as the foundation for advanced nursing practice. Previous RN experience does not expand one’s scope of practice as an APRN (Missouri Nursing Association, n.d.; Arizona Board of Nursing, 2009). Scope of practice also determines the minimum standard of competency and is governed by requirements for continuing education and professional accountability (Klein, 2005).
So, how do we make sense of all this?
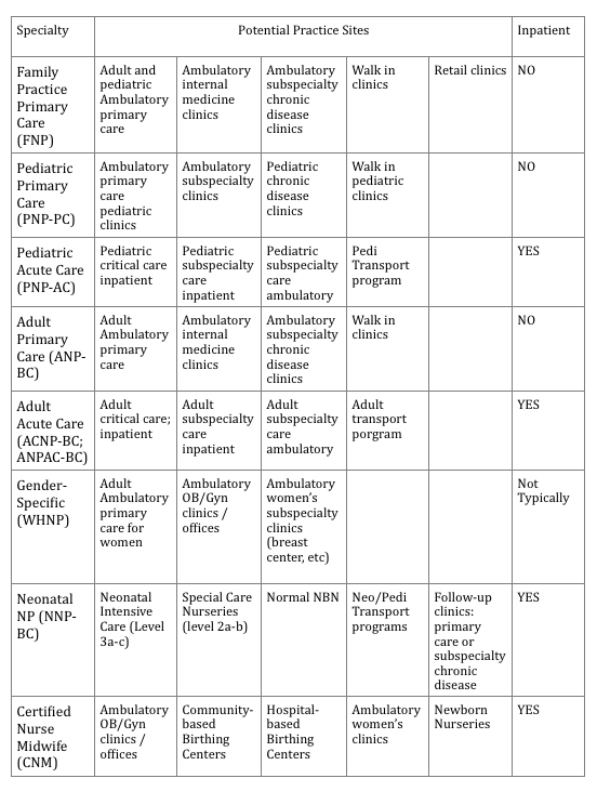
The following guidelines may serve to ensure that hiring directors/managers and supervising physicians are equipped with the knowledge necessary as they make recruitment and candidate selection:
References
- Arizona Board of Nursing. (2009). Registered nurses practitioner (RNP) practicing in an acute care setting. Phoenix, AZ: Author.
- Klein, T. (2005). Scope of practice and the nurse practitioner: Regulation, competency, expansion, and evolution. Topics in Advance Practice Nursing eJournal, 5(2).
- Missouri Nursing Association, Missouri Council on Advanced Practice Nurses of the Missouri Nurses Association. (n.d.). The status of advanced practice registered nurses in Missouri: A white paper.
- National Council of State Boards of Nursing. (2012). Changes in Healthcare Professions’ Scope of Practice: Legislative Considerations. Chicago, IL: Author